Type 2 diabetes increases an individual’s risk of Cardiovascular Disease (CVD). Trials have demonstrated the long term macro-vascular benefits of lowering glucose, as well as other CVD risk factors, in populations with established diabetes. As the diagnostic criterion for diabetes is a threshold on a continuous measure of glucose control, it has been hypothesised that targeting risk factors earlier in the disease trajectory may have even greater e↵ects on rates of complications.
Many nations have introduced programmes to diagnose diabetes earlier, including the NHS in England, where the Health Checks programme o↵ers individuals at ‘high risk’ diabetes testing. This will lead to a greater number of individuals being diagnosed earlier in the course of the disease when treatment decisions are less informed by evidence. Some of the potential harms of intensive treatment are likely to manifest early, while benefits will likely appear years later. Much of the literature relates to lowering CVD risk factors years after diagnosis or arises from studies conducted more than 20 years ago, which may not represent the e↵ects of managing risk factors intensively from diagnosis in contemporary care.
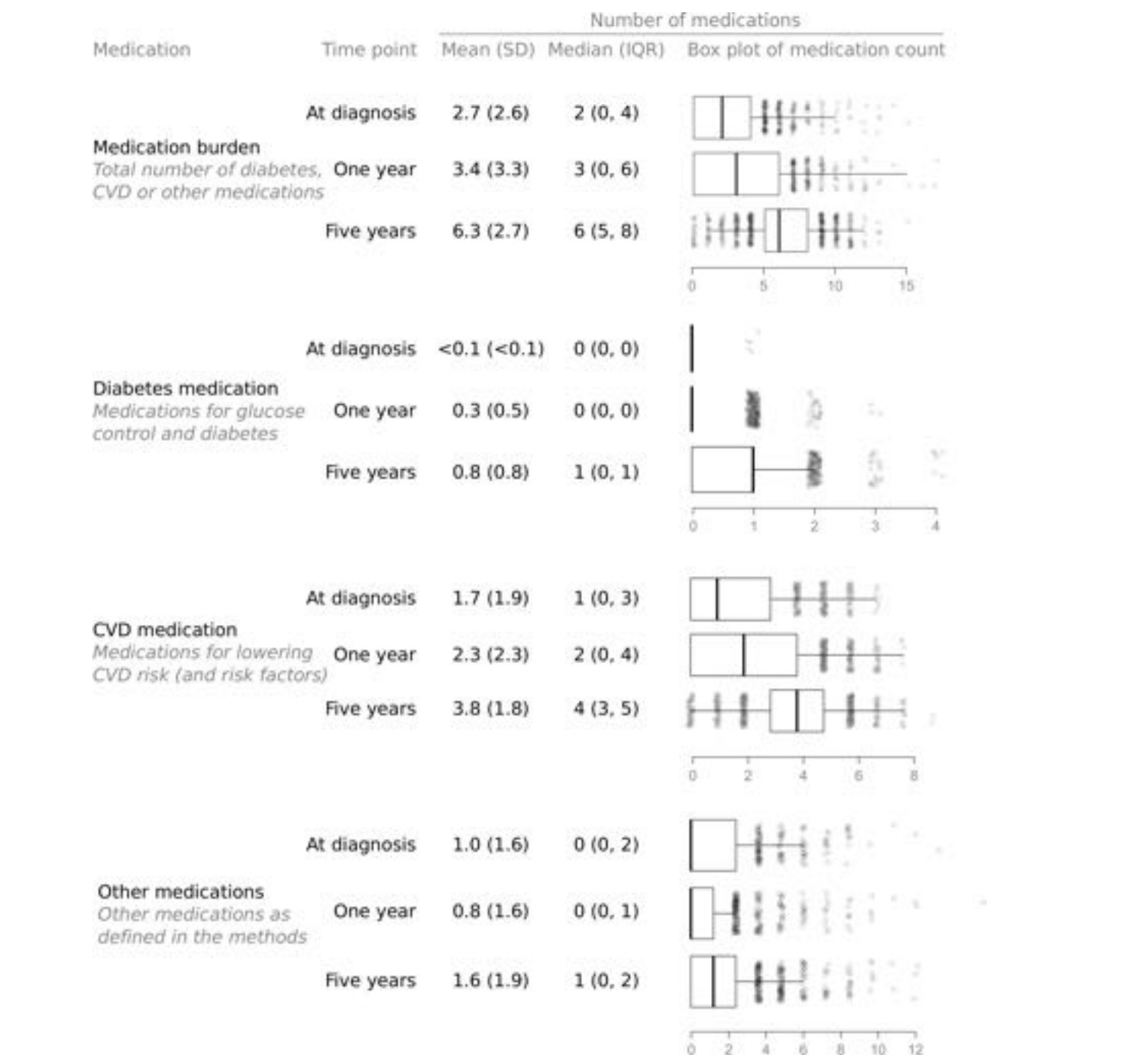
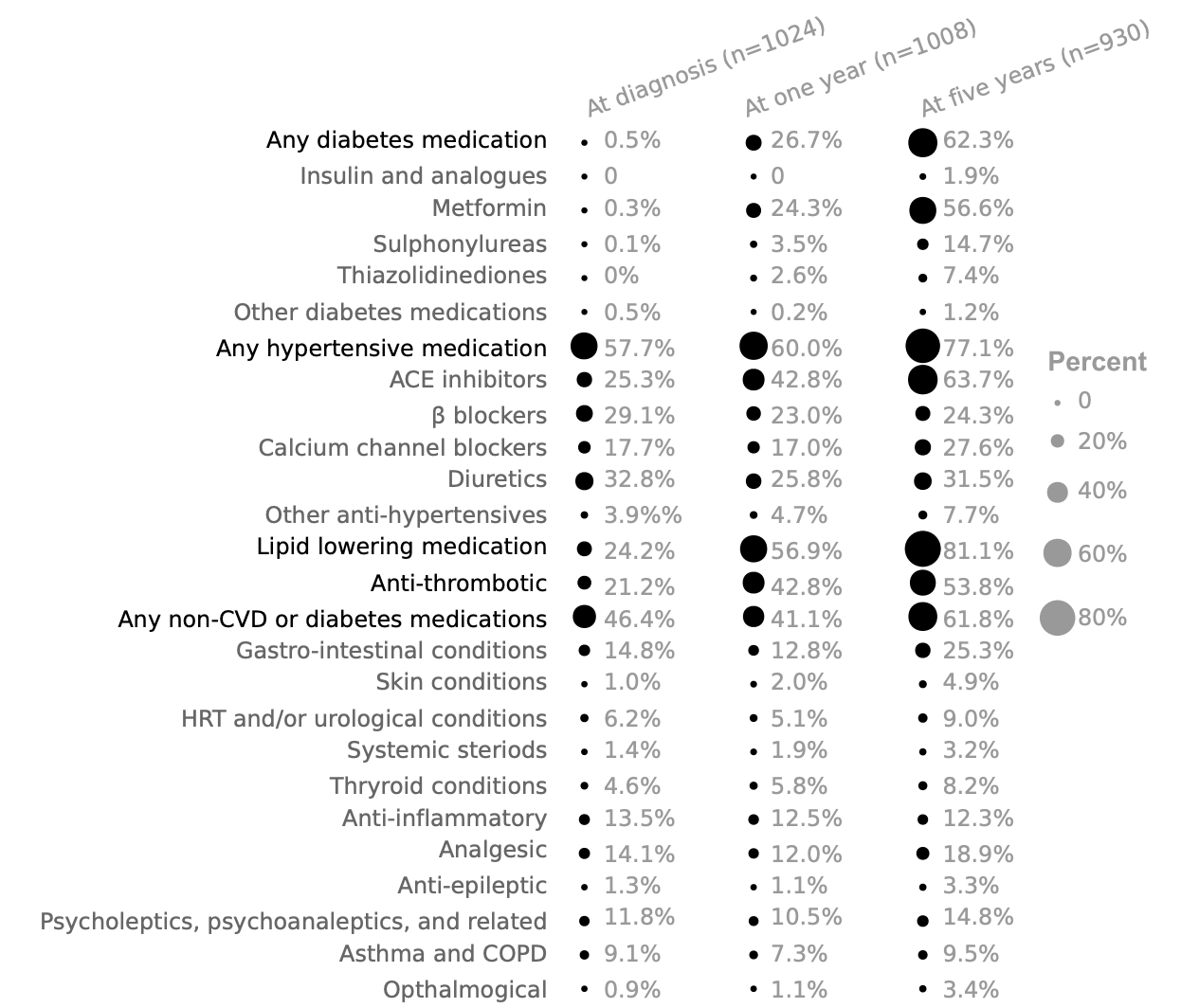
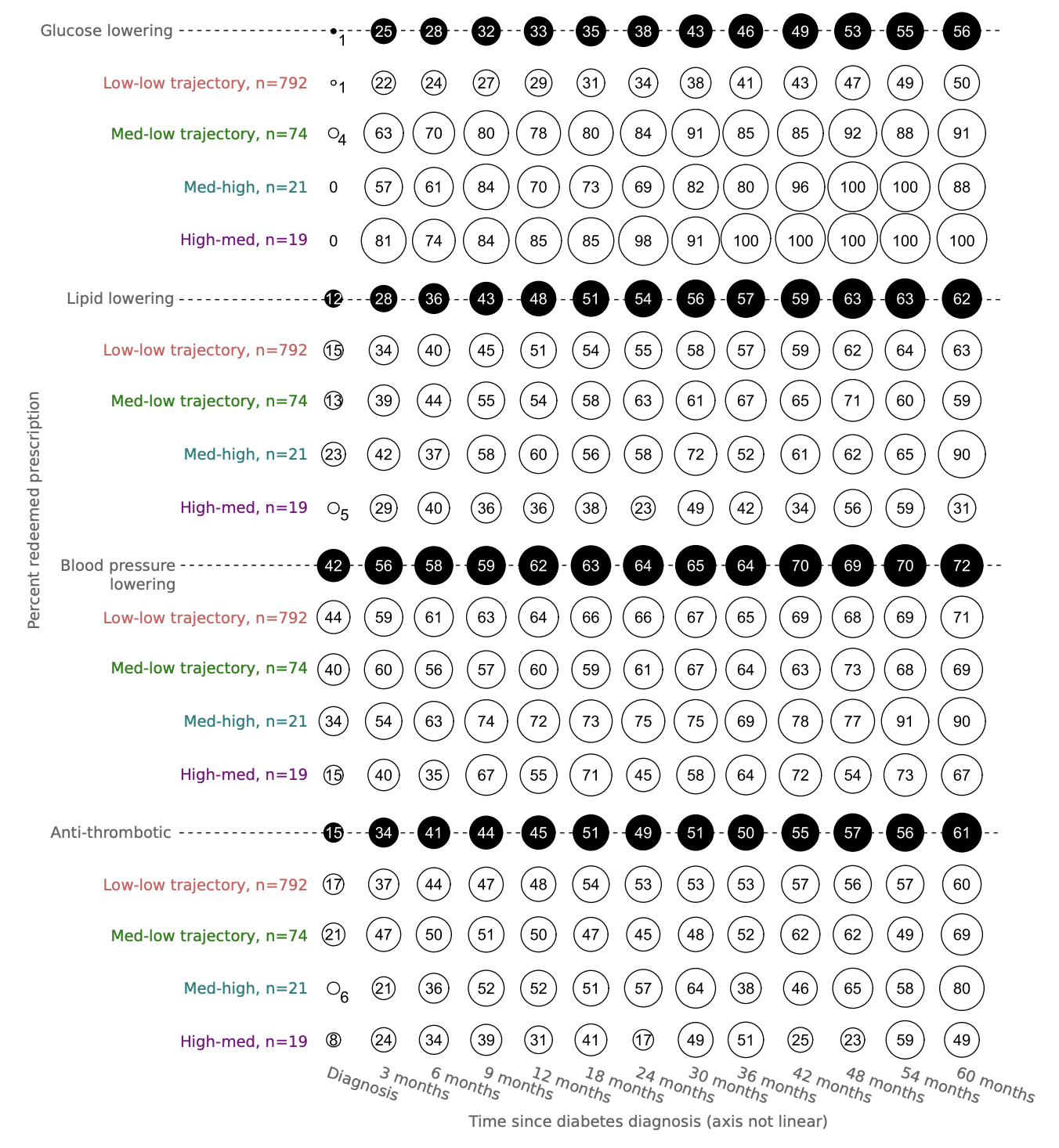
Firstly, I demonstrate that in a population with screen-detected diabetes there is a degree of pharmacotherapy burden at diagnosis, that then intensifies over the following five years.
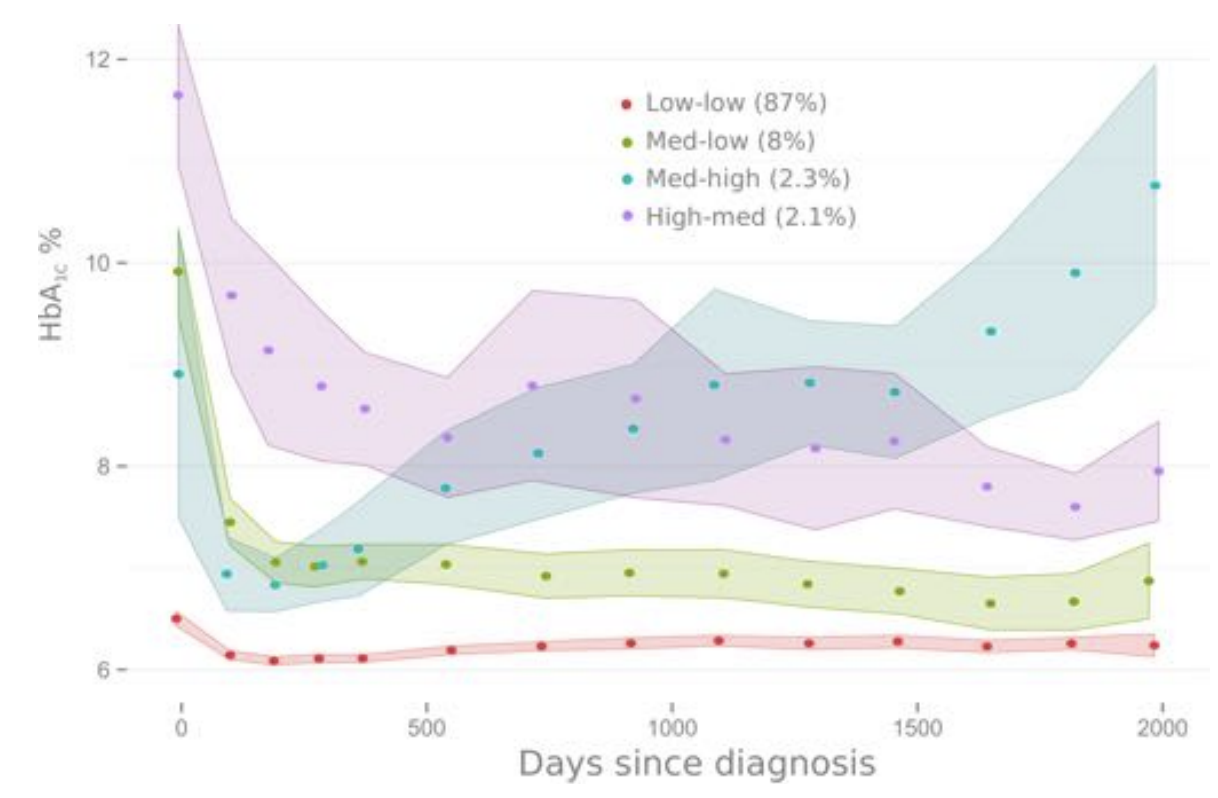
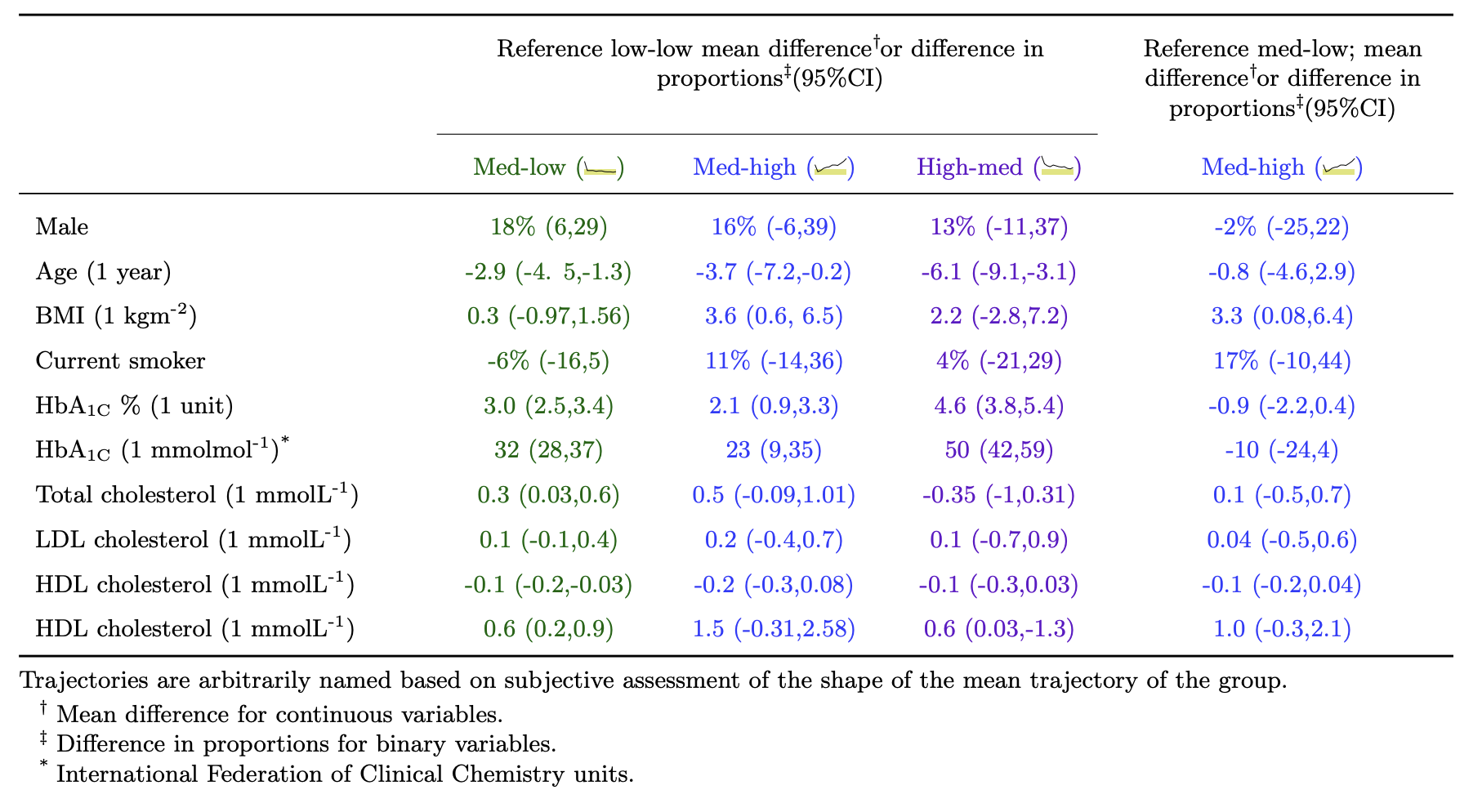
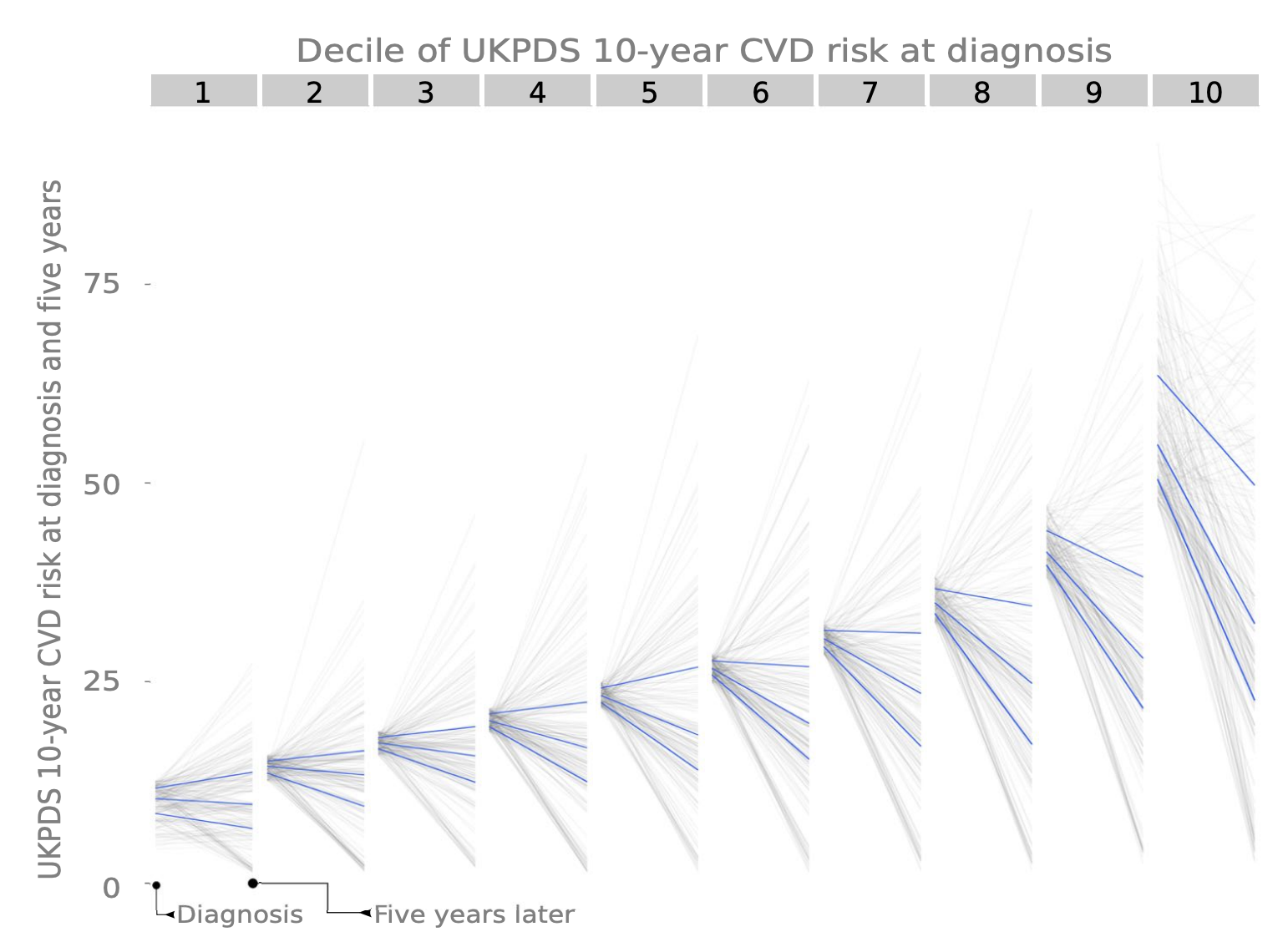
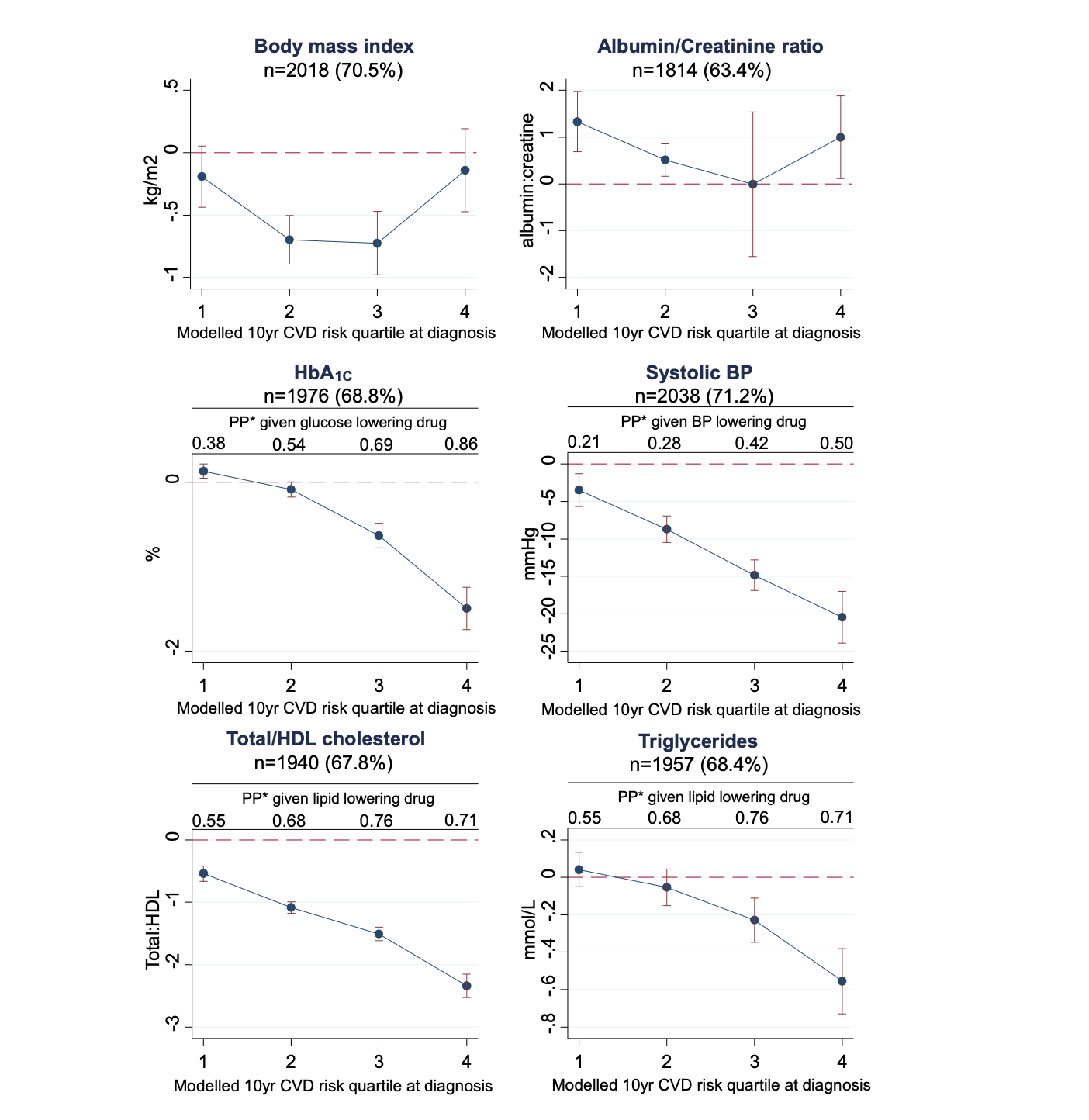
Secondly, I show that there is a large variation in glycaemic control and CVD risk factors after diagnosis at the individual level, which I have characterised and described.
Thirdly, I have shown that promoting intensive treatment from the day of diagnosis leads to improvements in cardio-metabolic health, and that increases in medication can decrease the modelled risk of a CVD event.
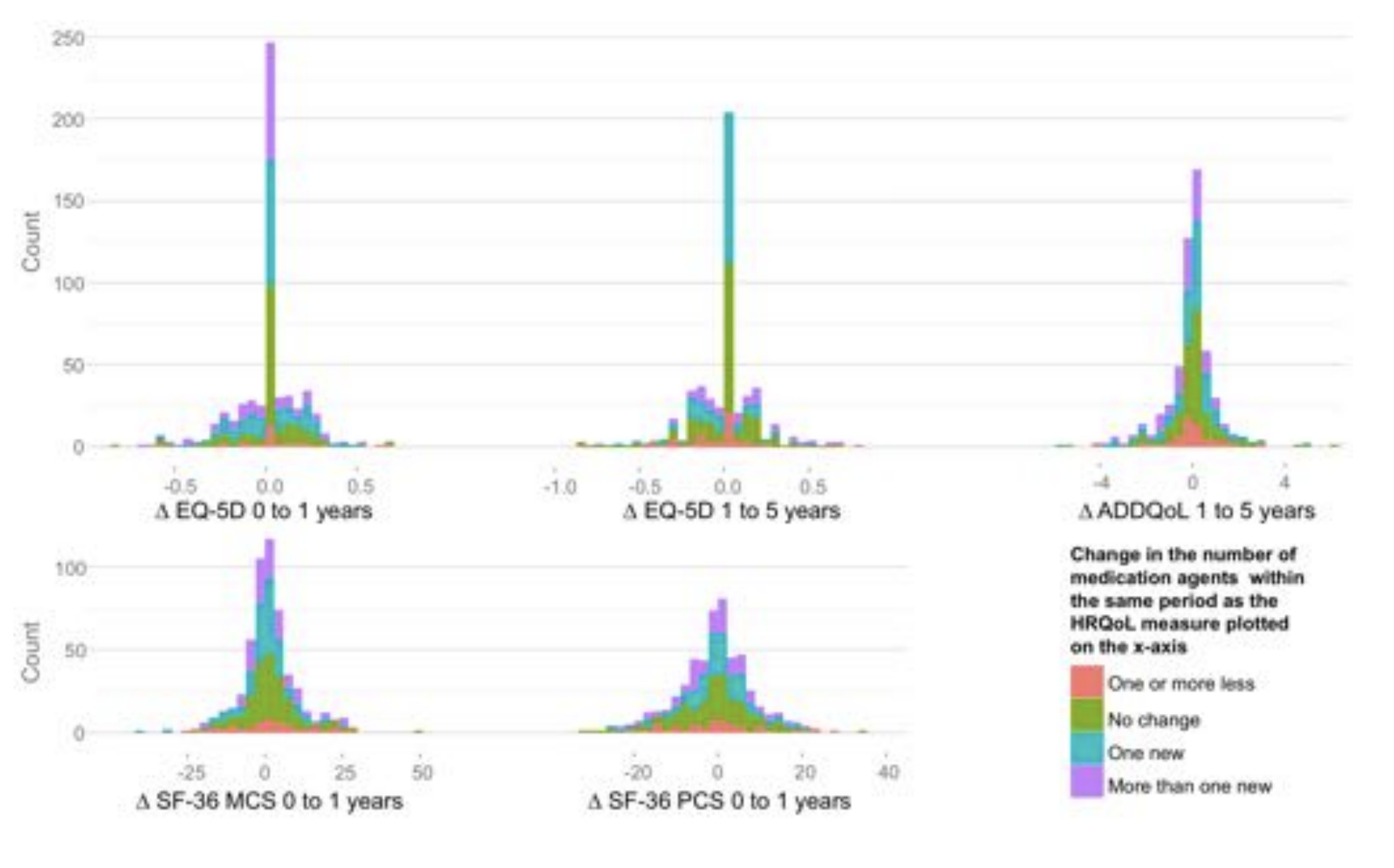
Lastly, I show that the risk reduction associated with intensification of pharmacotherapy is not achieved at the expense of quality of life.
In conclusion, type 2 diabetes is a disease intertwined with cardio-metabolic health, and actively approaching diabetes care as a multifactorial intervention to improve a cluster of cardio-metabolic risk factors via encouragement of lifestyle change supported by pharmacotherapy is likely to improve health. However, guidelines do not represent diabetes care at the individual level, and further research that both improves our understanding of individual variation and how to communicate these complex relationships will benefit our attempts to further personalise medicine.